About Those Skipped Heart Test Results
Harlem Hospital Center stands just three miles or so north of my home. I know the place from the outside glancing in, as you might upon exiting from the subway station just paces from its open doors. The structure seems like one chamber of its neighborhood’s heart; within a few long blocks’ radii you’ll find rhythms generated in the Abyssinian Baptist Church; readings at the Schomburg Center and artery-clogging cuisine at the West 135th Street IHOP.
So I was saddened to hear about the missed heart studies. Or should I say unmissed? No one noticed when nearly 4,000 cardiac tests went unchecked at the Harlem center, a public hospital managed by the city’s Health and Hospitals Corporation. The skipped beats began sometime in 2007.
According to the Times report, that’s when hospital administrators, hurting perhaps for doctors sufficiently skilled in reading echocardiograms, OK’d a process by which technicians scanning the images would alert the responsible physicians if they noticed abnormalities. Otherwise they stored the results – pictures of the heart’s contractions, wall thickness and size, valves and some large vessels – for review, later.
Usually when a person gets an echocardiogram there’s a reason. Mine, for example, was done before I received a chemotherapy drug, adriamycin that can affect the heart’s function and, another time, before I had a major operation – basically to make sure my heart was strong enough to handle the stress of surgery. Years earlier, I’d had an echo (as doctors sometimes call these tests) to evaluate shortness of breath I experienced while pregnant. I like echocardiograms, as cardiac imaging methods go, although I must admit I find the blobby representations cryptic if not frankly rorschachian. These tests rely on ultrasound, the same technology we routinely use to examine unborn fetuses by projecting and canvassing sound waves. There’s no radioisotope or x-rays. Not even a magnet’s involved.
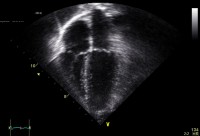
What generally happens is that after the procedure a doctor, usually a cardiologist, inspects the images and provides a written assessment. Ideally, the test report reflects the reason for doing the procedure. So if a teenage soccer player has an echo to evaluate an episode of fainting on the field, the physician-reviewer would focus on structural heart abnormalities associated with sudden death in some young athletes. Sometimes the studies reveal enlargement of the heart; this can occur in alcoholics, in people with chronic forms of severe anemia like sickle cell disease, and in other conditions. For patients with atrial fibrillation – a disorder in which the heart flutters irregularly – doctors might look to see if there’s clot inside the heart’s walls that might, unmitigated, migrate through the arteries to the brain. Echocardiogram can assess the heart’s condition after a heart attack or in congestive heart failure. They can visualize holes in the heart chamber walls of infants, lapsed valves and more.
The Times story indicates that doctors didn’t review images for over half of the echocardiograms performed at Harlem Hospital since 2007. The medical center, staffed by doctors from Columbia University, had six attending cardiologists and six fellows in 1999, according to the paper. Now the hospital has only three full-time cardiologists and lacks a fellowship program. The hospital runs approximately 2,500 echocardiograms each year. Among those 4,000 patients whose tests went unread, some 200 have died since the time of the procedure. Hospital officials say it’s unlikely that any deaths are attributable to the lapse.
Since the story emerged last week, a squad of doctors has been scrambling to review the images. Heads rolled at Harlem Hospital: the clinical director was fired and the medical director has been demoted. An investigation, led by Dr. John N. Morley of the State Health Department, is underway. The press, or at least my local newspaper, is all over the matter.
So what’s to be learned from this oversight? My take’s two, so far:
1. It appears that at least some physicians working at Harlem Hospital felt it was understaffed and that they were too overworked to meet their clinical responsibilities, and that the administration did not adequately address their concerns. And while Health and Hospitals Corporation has indicated this problem is unique to that particular department – the echo lab – at one hospital, I’m not convinced.
Having worked for years in hospitals where cardiologists, gastroenterologists, hematologists and even pathologists spend much of their time putting out fires, so to speak, it’s scarily easy for me to envision how non-urgent tests could pile up without review. When hospitals operate with money as a bottom line, the difficult work doctors do doesn’t get easier. So we might blame individual physicians for not signing those reports. But I’d take the system to task, and not just at one Harlem hospital.
2. No one’s mentioned the patients’ role in all of this, which seems strange to me. These days, we expect that most patients will enter into discussions with their physicians about what tests they need done. Maybe at a medical center like Harlem Hospital, which serves a relatively poor population, the expectations differ regarding patients’ involvement in medical decisions. But if that is the case, those separate standards reflect another problem – of poor communication between physicians and their patients – equally demanding of our attention.
Lastly, as I’ve said previously here and elsewhere, we waste a lot of medical resources by ordering procedures without thinking. If a person undergoes a medical test there should be a reason for it, sufficient that either the doctor or the patient cares enough to find out the results.
What about the physicians who ordered the echos? Wouldn’t he/she look for the results?
Meagan,
I agree completely that doctors shouldn’t order tests if they’re not going to check the results.